Assessment is completed
What is:
Upon admission, every four hours, more frequently as patient acuity dictates.
I and O = Hourly
Changed on Wednesday and Saturday
What is IV tubing, extension tubing and pressure caps (unless more frequent change is expectation)
Must be completed by due date or my Educator will pull her hair out!
What are Pathway modules
3 times Clinician Documentation should be documented?
What are Consults, Donor Network Communication, and Medical Examiner
Completed with 12 hours of admission
What is the adult admission history/assessment including home medications
Suction Cannisters and tubing, including Yankauer should be changed
What is every 24 hours
Vital signs are assessed
What are Q1H or every 15 minutes if the patient is receiving vasoactive medications and with medication changes.
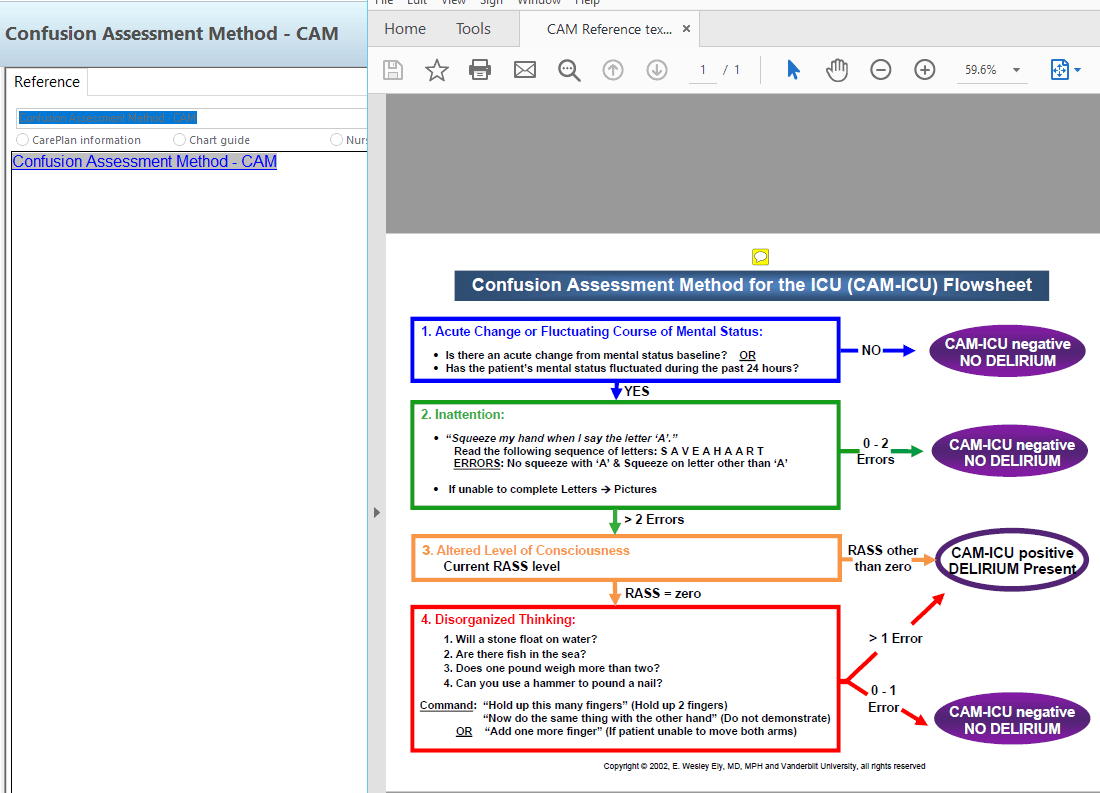
Both RASS and CAM have
What is a reference in Cerner.
The source of truth for particular skills
What is Elsevier Clinical Skills
Documentation required for pain and sedation
What is:
Pain
Every four hours and after pain medication administered
Every hour if on a continuous analgesia infusion, 15 minutes after any titration, & PRN
Match titrations with order
RASS
If patient on sedation, every two hours and with titrations
If patient is not on sedation, every four hours
Match titrations with order
Valuables and patient belongings are assessed and documented
What is upon admission and each patient change in location.
Placed in dirty utility room if kitchen car is not available
What are dirty patient meal trays
If it is assessed, it them must be
What is DOCUMENTED
All critical care patients are considered
What is a high fall risk
ALS and BLS are completed
What is Quarterly
Documented within 45 minutes and where?
What is a Critical value result and is documented on an AdHoc Critical Value Result Note
How often the shift screening is completed
What is at least every shift
Kept in each room boom basket
What are 2 suction tubing's; 2 yankauers, 3 BP cuffs (S, M, L,), EKG electrodes, O2 sat Probe.
Mobility Screening assessment is completed
What is every shift
Per the Dignity Health Early Progressing Mobility Protocol
Post Anesthesia Recovery vital signs (direct to ICU)
What is:
Every 5 minutes x3
Every 15 minutes x2
Then as ordered
Medication reference content
What is Lexicomp
The patient's weight
What is documented daily
Documented under Bony Prominences upon admission to ICU
What is 2 person skin assessment
A green lift sheet (if needed), flat sheet, dry-flow chux, and SCDs
What are standard linens for bed zeroing
RN to RN hand off is completed at the patient's bedside and includes
What is:
Update white board during handoff.
Verify patient arm band (s) are accurate to include: fall, allergy, DNR.
Neurological assessment to be completed simultaneously by oncoming and off going RN’s.
Central line dressings are
What are changed every Wednesday and PRN if soiled or compromised.
Aid in decision making under a given set of circumstances and are based upon norms/standards of practice.
What are Policies
Documentation required for Non-Violent Restraints
What is:
Every 2 hours on even hours in monitor and assess sections under assessment
If patient is off the floor (i.e. OR, Cath lab), document in restraint charting under Additional Information section the time patient left ICU, where they went to, and time returned to ICU
Plan of Care for Restraints documented every shift
Add restraint education to education section
A non-violent restraint order every calendar day (ideally put in at Midnight)
What are specific patient/family education provided upon admission. (Name at least 4)
What are Falls, Infection (CLABSI, CAUTI, SSI) Smoking, and Handwashing. East Valley admission, anticoagulants, restraints and new medications. (Specific patient education documents to be placed in Dignity Health folder at bedside.)
Patient room and nursing station should be
What is left clean and orgainized for the next shift.