Which nerve supplies the gluteus minimus, gluteus medius and gluteus maximus?
Inferior gluteal nerve (maximus)
Superior gluteal nerve (minimus and medius)
Bonus points function of each muscle:
Dr. Bartnick is seeing a patient in her clinic presenting with progressive weakness and paresthesia for the past 3 weeks. The patients wants to provide a detailed hx but Dr. Bartnick has no time to waste, being chief and all. She says and I quote, "Why would i listen to your words when the journey towards the truth can be so much more fun". With a smirk she proceeds to electrocute and stab the patient with a needle AKA performs a NCS/EMG.
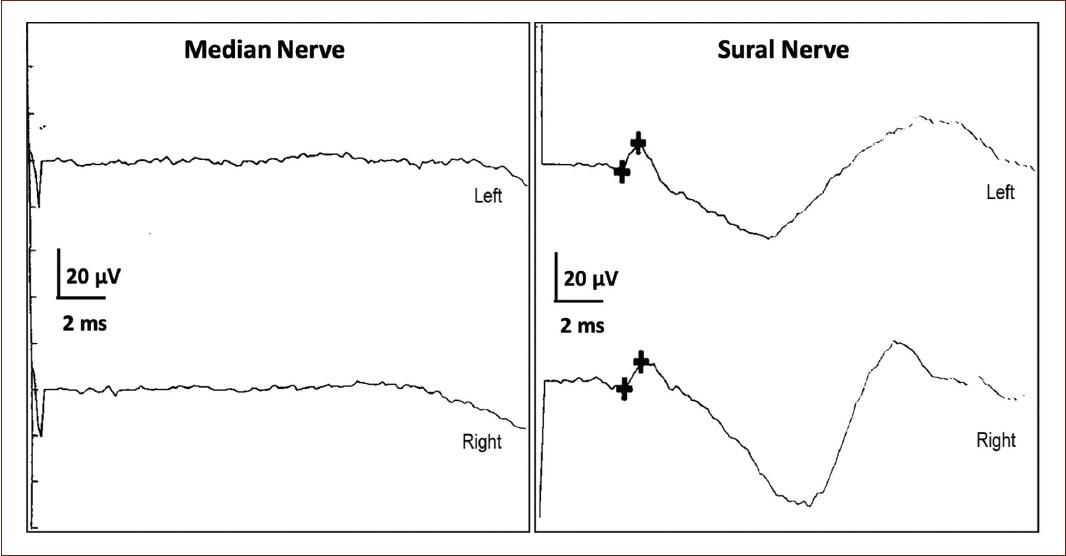
The test shows absent H responses & absent F waves, some of the waveforms from the study are shown below. The most likely diagnosis is...

What is AIDP
Earliest sign on NCS: Delayed/Absent or impersistent F waves or H reflexes (reflecting proximal demyelination/ note AIDP starts at root level as polyradiculopathy).
Motor NCS show prolonged distal latencies and conduction block or temporal dispersion. (50% have these at week 2 and 85% by week 3)
Lae findings: Conduction velocities on MCS become slow. Sensory studies (classically) show a so called "sural sparing pattern" i.e the upper extremity nerves have absent or reduced SNAPs but sural SNAP is normal (AIDP preferentially affects small diameter myelinated fibers)
Reduced/absent SNAPs in the UE with normal sural SNAPs (sural sparing) highly specific for diagnosis of AIDP
Discuss the difference in clinical presentation of a L5 radiculopathy versus a common peroneal neuropathy.
Clinical findings can aid in determining the etiology of a patient’s condition. L5 radiculopathy and peroneal neuropathy can both present with weakness of the foot dorsiflexors and toe extensors.
L5 radiculopathy may present with weakness during foot INVERSION whereas peroneal neuropathy will not.
Additionally, reflex changes at the patella, medial hamstring and Achilles tendon can distinguish a L4, L5 or S1 radiculopathy from a common peroneal neuropathy.
Sensory changes to light touch or pinprick may not improve the clinical picture as dermatomal patterns and peripheral nerve distributions can have much overlap and sensory evaluation may be prone to subjective bias.
Finally, adverse nerve root tension, including femoral nerve stress test and straight leg raise can indicate a lumbar nerve root involvement which is absent during peroneal neuropathy. On the other hand, passive or forceful ankle inversion tensions the peroneal nerve which may reproduce symptoms of a peroneal neuropathy.
Name the gene mutation for each of the following forms of Charcot Marie Tooth disease and the mode of inheritance
- CMT1a
- HNPP
- CMT1X:
Bonus points if you know this:
CMT2A: mode of inheritance, type of neuropathy
CMT4: mode of inheritance
Autosomal dominant: CMT1 and CMT2
Autosomal recessive: CMT 4
X linked CMTX
CMT1-most common type of CMT (40-50%) (6 subtypes) all are demyelinating hereditary motor and sensory neuropathy with nerve biopsy findings of demyelination and onion bulb formation.
*CMT1A: MC CMT overall. 70-80% of CMT1 cases. Associated with a duplication on PMP22 gene on 17p.
* CMT1b MPZ gene on chromosome 1 (more severe, 10% of CMT1 cases)
* HNPP: AD. Deletion in PMP22 gene on chromosome 17p. Clinically present w/ recurrent episodic painless mononeuropathies in adolescence or young adults (variable)
CMT2-axonal form in which motor CVs are normal or near normal and nerve biopsy reveals axonal loss without prominent demyelination. AD inheritance begins later in life 2-3rd decades, foot/spinal deformities are less prominent-similar clinical features except peripheral nerves are not enlarged and upper extremity involvement, tremor and general arreflexia occur less frequently.
CMT4 Autosomal recessive
Discuss the stretch reflex.
Hitting a tendon with a reflex hammer causes a stretch to be applied to a muscle, which is detected by the muscle spindles. Due to the stimulation of the muscle spindles an excitatory impulse is sent through Ia afferent fibers (sensory nerve) to the alpha motor neuron in the spinal cord which then fires and causes contraction of the muscle (a monosynaptic pathway).